The best approach is a secure, standardized platform that supports multiple data sources and reporting needs. Azara enables efficient data sharing that aligns health plans and providers around common goals.
Health Plan Solutions
Azara empowers health plans to achieve better outcomes for their members through a proven, scalable technology platform.

Azara delivers timely, actionable clinical insights that facilitate collaboration with provider organizations.
This enables health plans to work hand-in-hand with providers on critical initiatives like improving clinical quality, recapturing risk, and driving performance improvement. By equipping providers with up-to-date, actionable information, Azara fosters a collaborative environment where all stakeholders can work together to monitor, track, and improve quality, cost, and utilization outcomes for the entire member population. Additionally, Azara optimizes risk gap closure and streamlines clinical evidence capture.
Azara seamlessly integrates with existing care workflows by ingesting claims and clinical data from various sources. This unified dataset enables member-focused programs to optimize quality measures, identify and work risk and care gaps, and precisely identify and target high-risk members through risk stratification – all within the unified Azara DRVS platform.
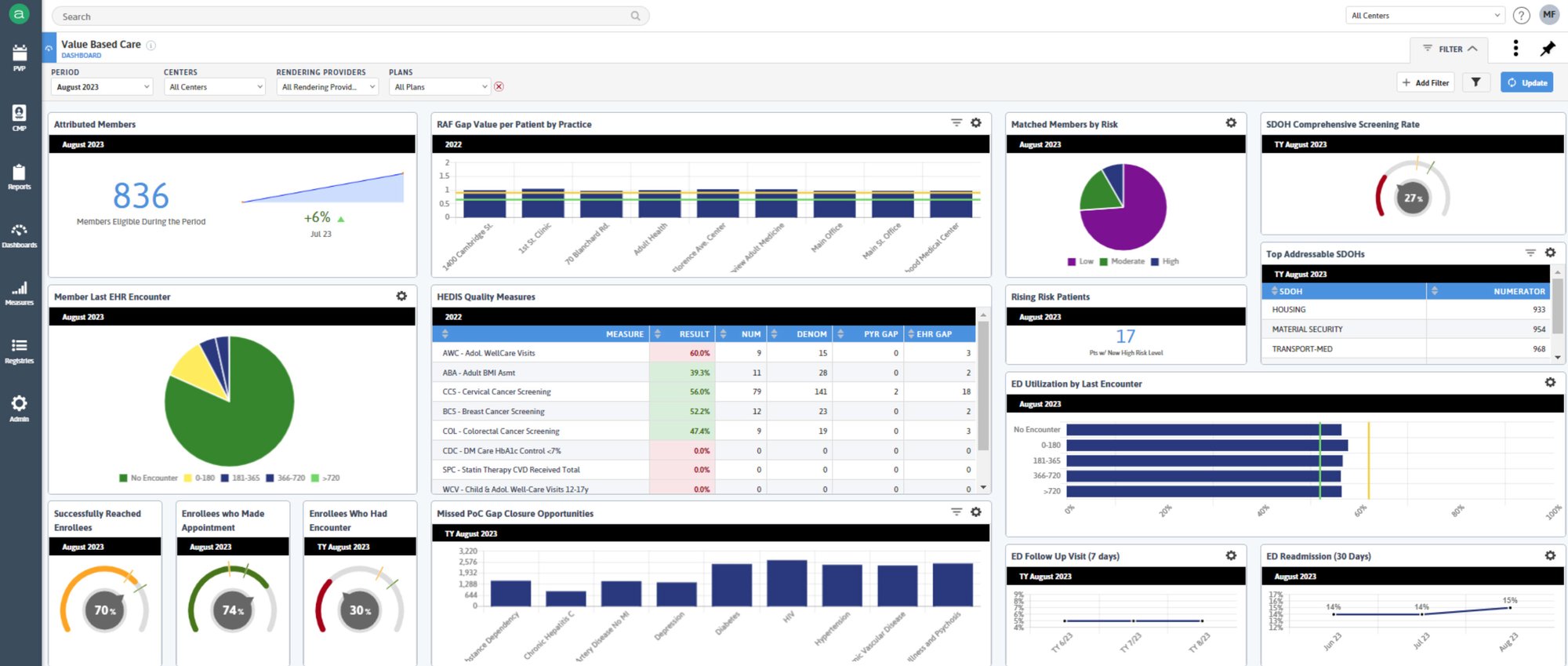
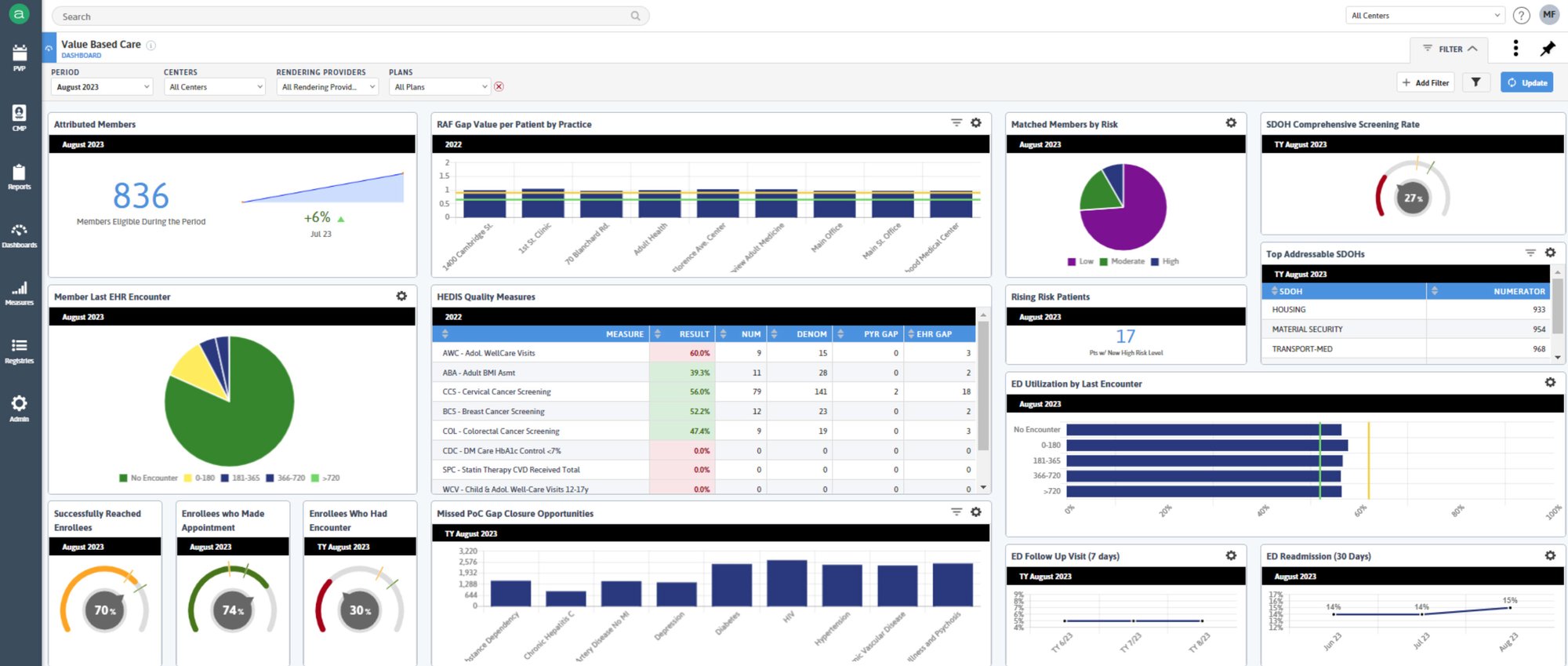
Azara DRVS further supports value-based care success with an experienced Clinical Transformation team and a comprehensive library of over 300 measures – including over 50 certified HEDIS® measures, MSSP ACO eCQM/Medicare CQM, and a broad range of clinical quality measures, covering Medicare, Medicaid, and commercial contracts.

Health plans use Azara solutions to engage with providers and members – improving care by enabling plans to:
Unify member insights by incorporating aggregated, standardized supplemental data directly from providers – empowering the health plan's teams with a comprehensive and timely understanding of members' conditions and risk factors.
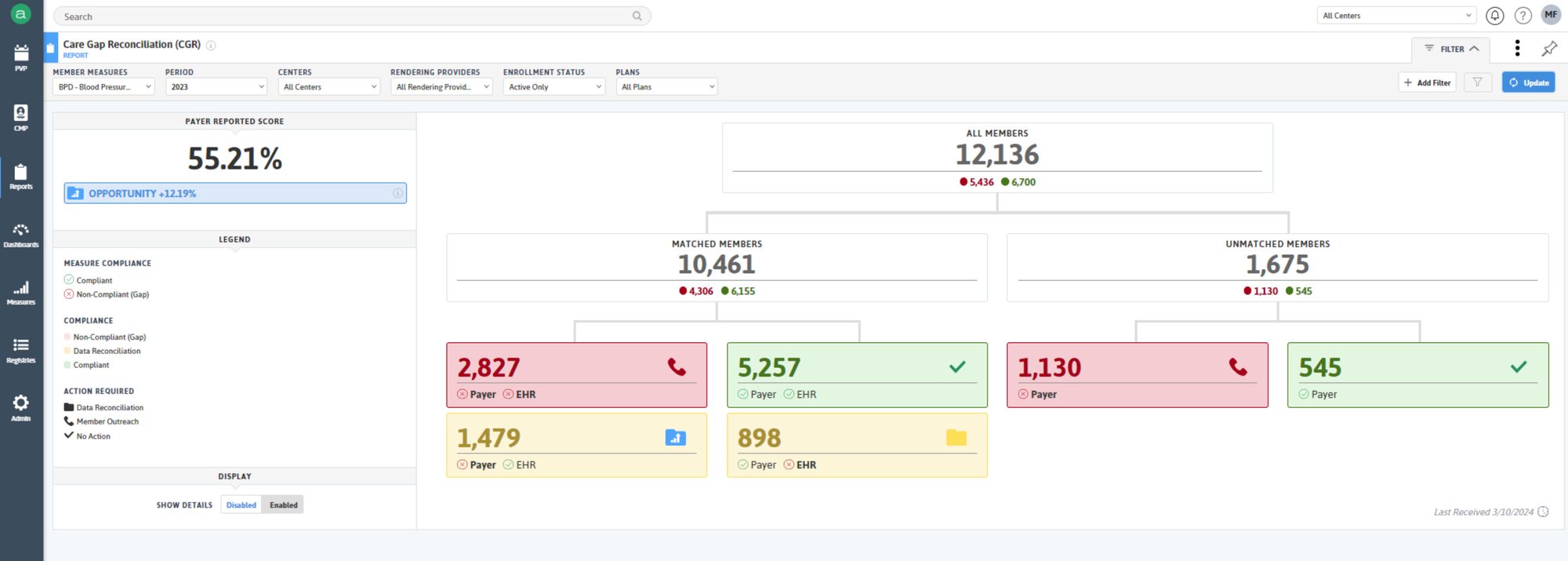
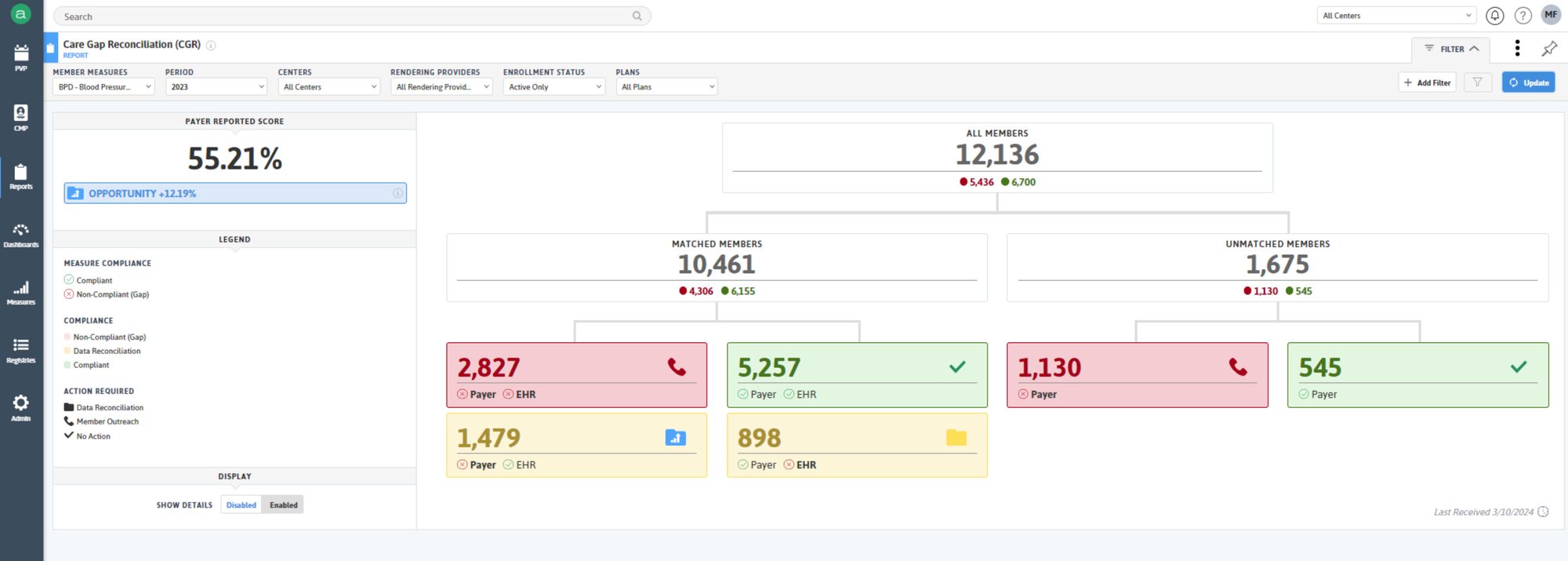
Significantly reduce wasted time and effort by closing care gaps with Azara's automated care gap reconciliation which seamlessly matches payer-calculated gaps against EHR data – revealing the true status of gaps and ensuring resources are focused on the issues that
matter most.
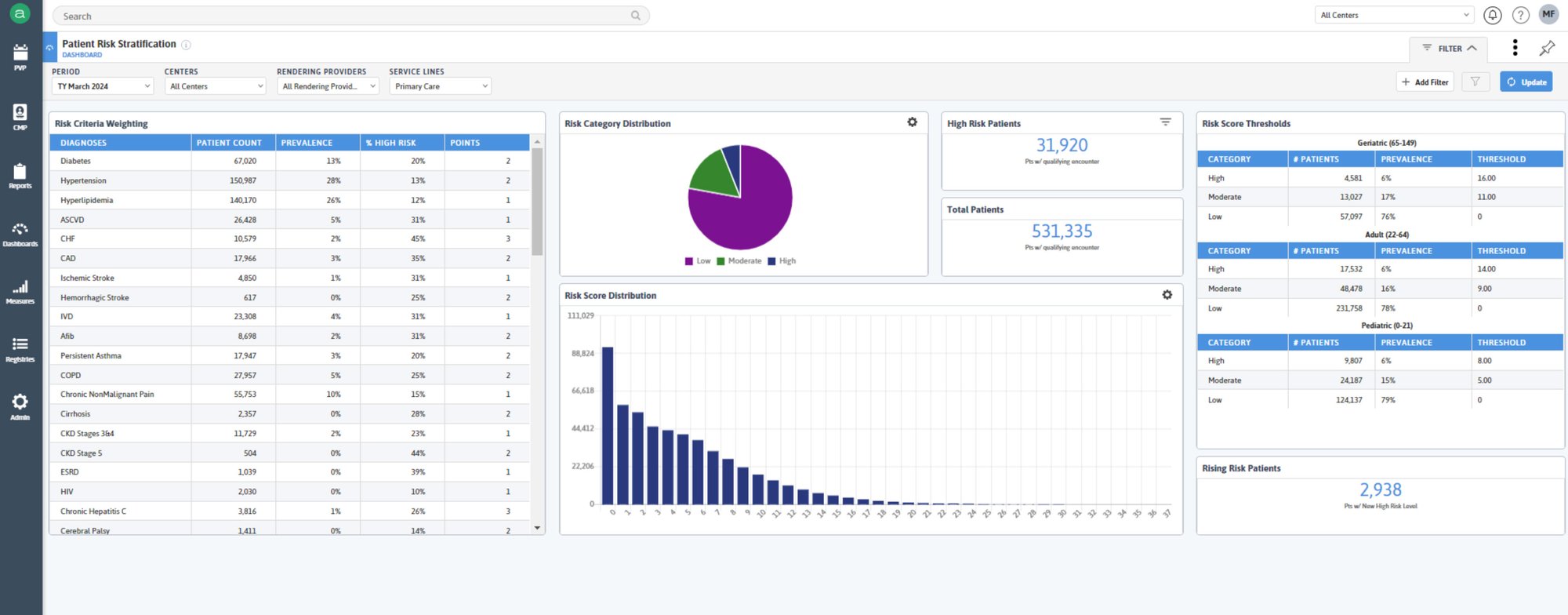
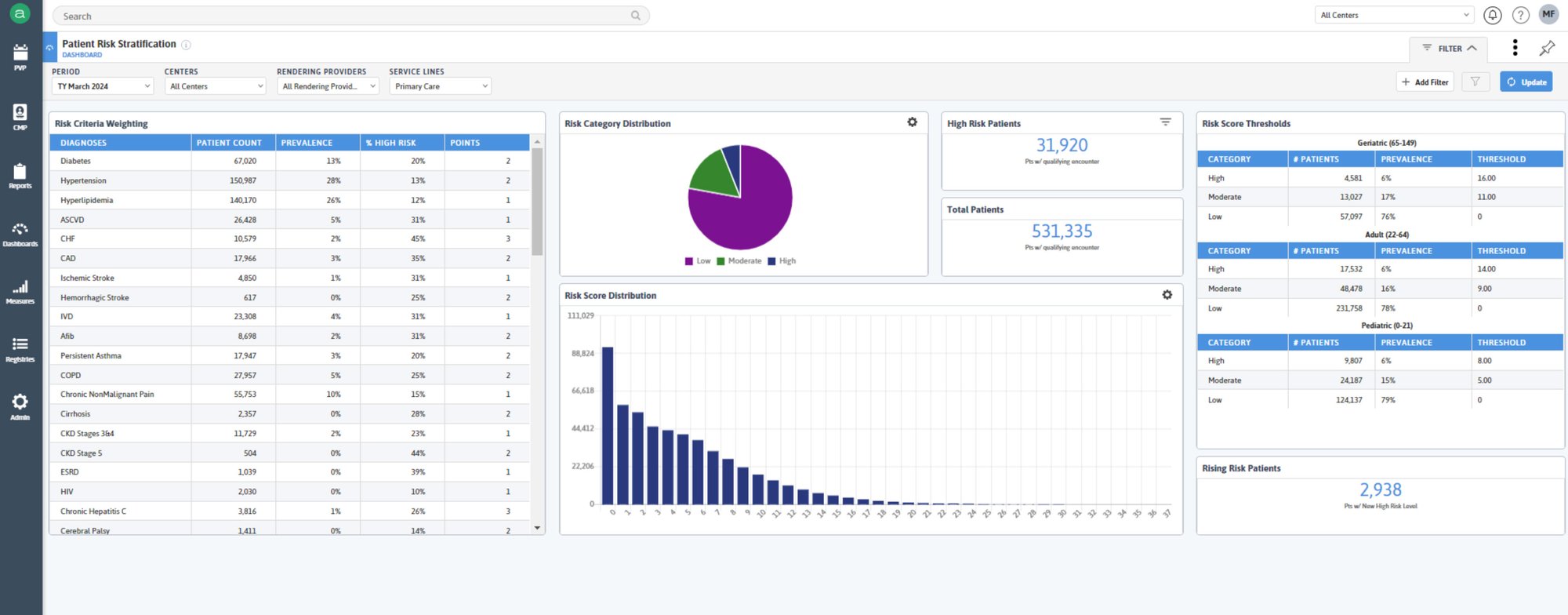
Access real-time risk stratification to continuously identify and address potential member health issues.
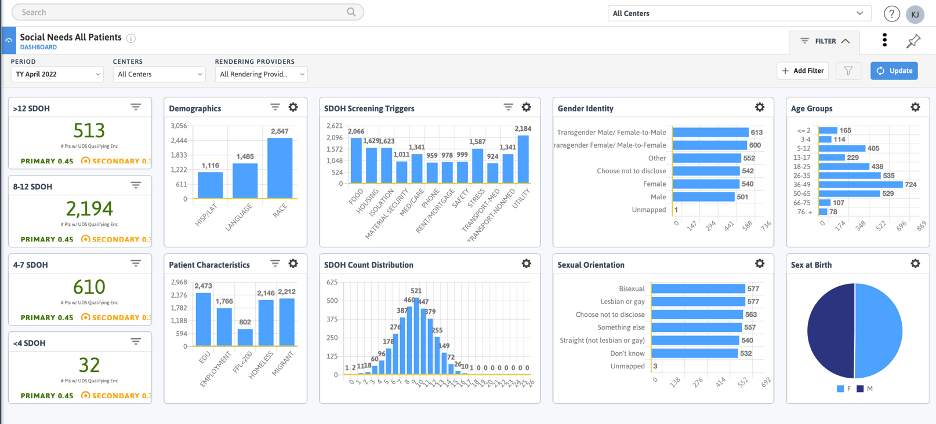
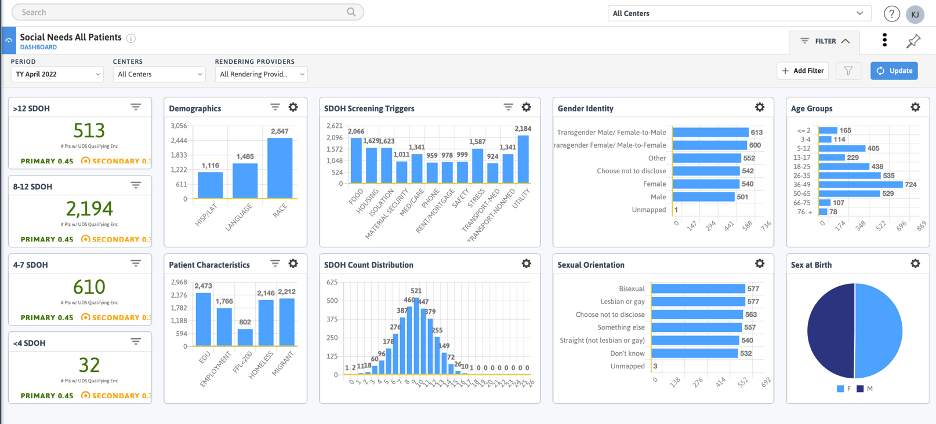
Leverage expanded clinical insights, including social determinants of health (SDOH) and demographics to optimize HEDIS measure performance and facilitate risk recapture.
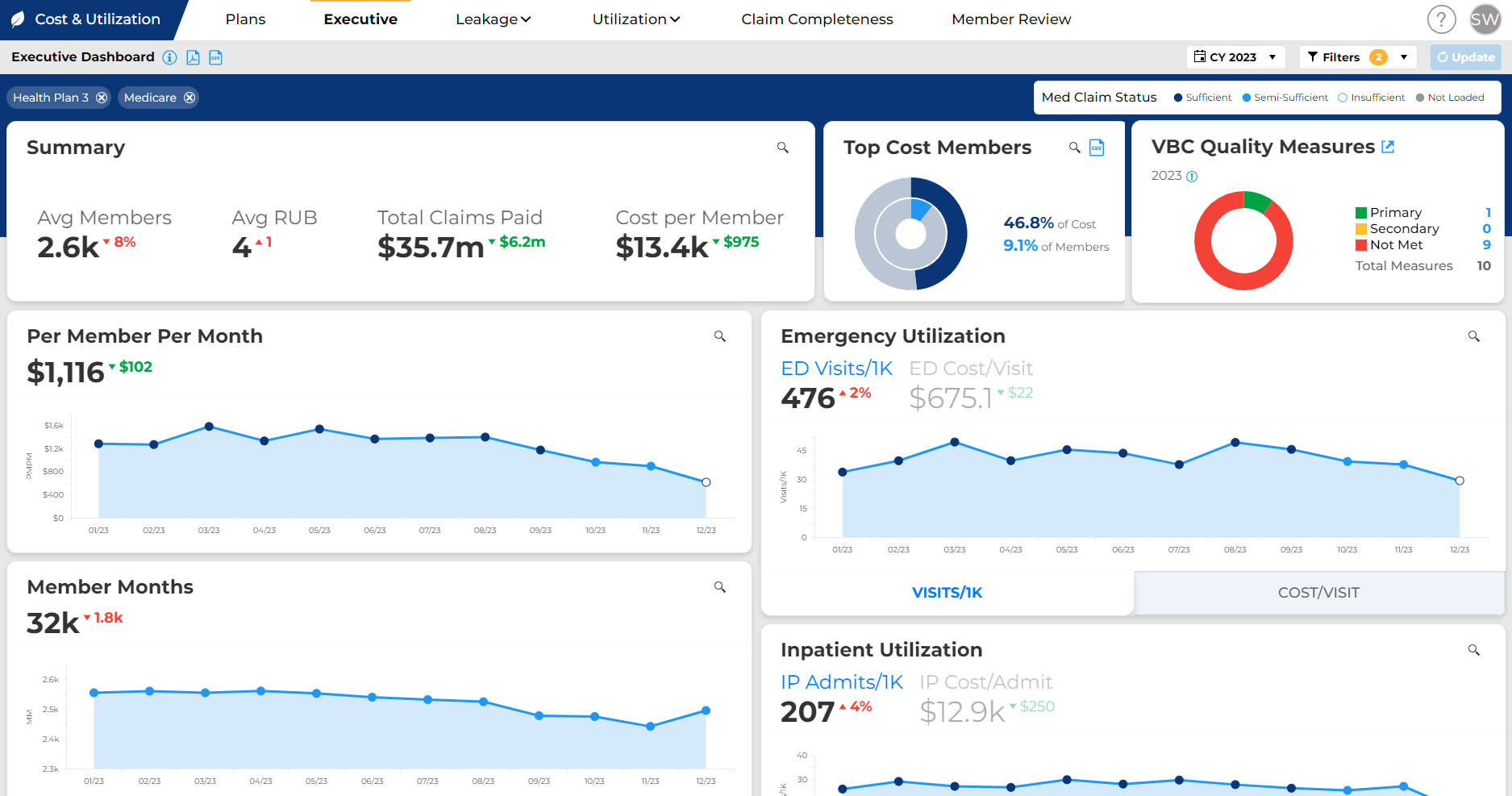
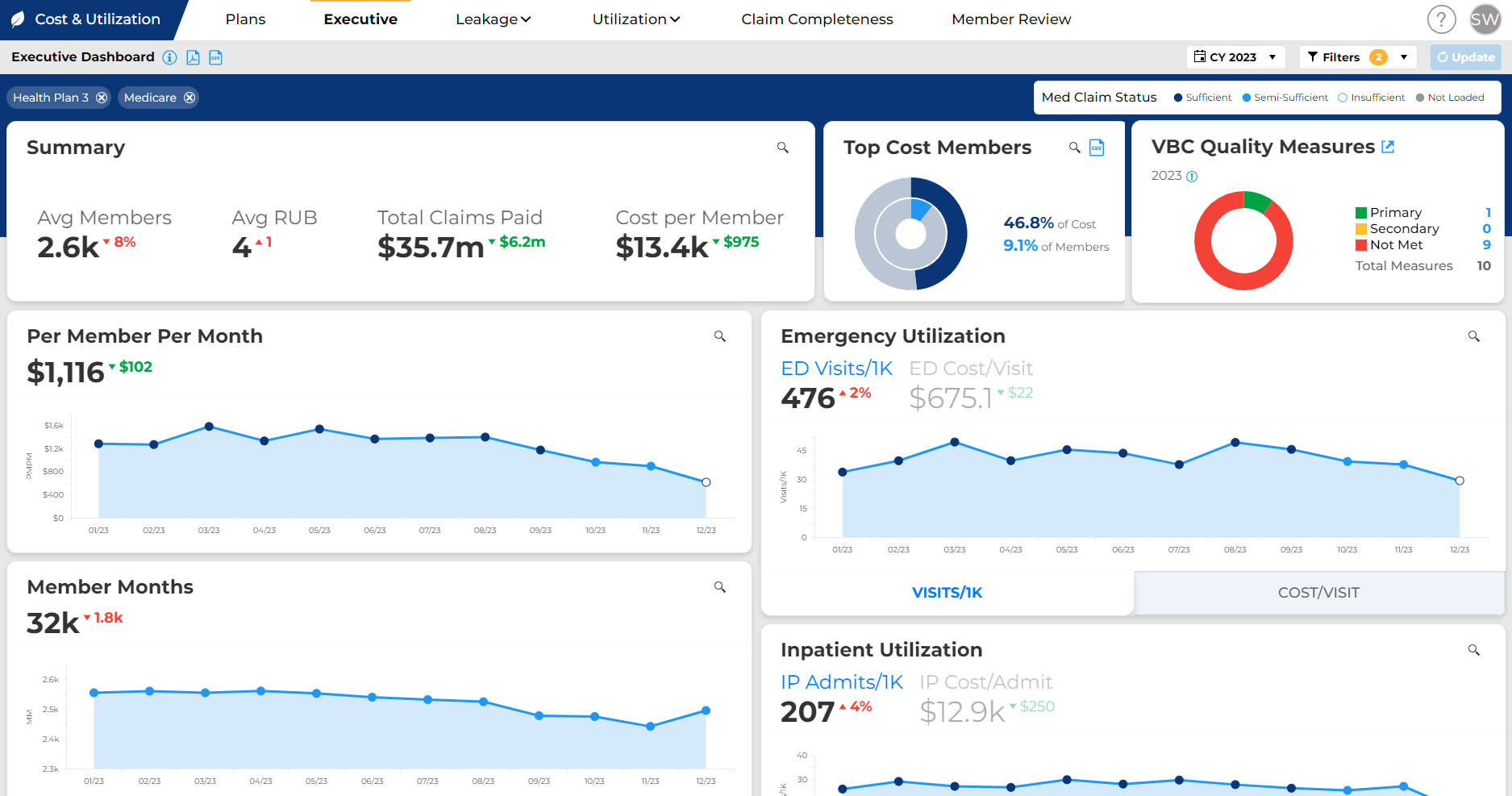
Gain granular insights into cost and utilization drivers throughout the network, enabling targeted interventions to optimize performance at the network, practice, and provider levels.

Azara DRVS empowers users to navigate the complexities of value-based care with a highly configurable and feature-rich platform, which includes:
Intuitive Dashboards
Uncover performance insights at a glance. Intuitive dashboards offer a clear, high-level view and empower users to drill down seamlessly into specific data sets for deeper analysis.
Innovative Dynamic Cohorts
Identify members who need specific services and automatically align members to relevant programs or interventions based on daily updates to their health data.
Data Activation
Equip health plan teams with actionable clinical insights while also delivering plan data to providers directly at the point of care. This real-time access to critical member data significantly boosts risk recapture and care gap closure rates.
Value-Based Care Success
Azara's deep analytics provide a granular view of performance at the network, practice, and provider levels, enabling data-driven decisions for continuous improvement.
NCQA Data Aggregator Validation
Azara Healthcare was part of the first cohort organizations which earned Certified Data Stream status in 2021 for NCQA’s Data Aggregator Validation Program - the highest level of certification offered by the National Committee for Quality Assurance (NCQA).
Validated data flows promote trust in aggregated clinical data. They support adoption of value-based contracting by making many of its core features more workable. This also eases the quality measurement load - validated data streams are uniquely accepted as standard supplemental data in HEDIS® audits. This means no primary source verification is required for HEDIS reporting when health plans report data from validated sources.
Validated data flows are an important, early step on the pathway to a digital measurement ecosystem.
Frequently Asked Questions
What should health plans look for in a population health partner?
Health plans should look for scalability, interoperability, strong analytics, and proven experience supporting diverse provider organizations. Azara offers a flexible platform designed to meet these needs.
Can Azara help us support multiple provider organizations with different reporting needs?
Yes. Azara’s platform supports configurable reporting and analytics, allowing health plans to meet the unique needs of different provider organizations without creating separate systems.
Additional Resources
MARKET REPORT
Download our findings report to learn what is slowing VBC progress for providers and health plans
CASE STUDY
Points of Light 2023 - Improving Equity in Healthcare Access through Improved Data Exchange
SUCCESS STORY
Regional Louisiana health plan partners with Azara Healthcare on chronic disease management for value-based innovation in primary care



