With one in three primary care visits resulting in a referral, the referral represents a critical inflection point in a patient's care journey1,2. The success of that referral is dependent on a high-functioning, synergistic collaboration between patients, providers, and specialists. Given so many variables, practice staff may feel as though much of the process is out of their control. However, management insights can offer practices perspective into their communication strategies, practice workflows and coordination, and resources available within the network, which together can be harnessed to better support patients throughout their referral journey.
This delicate codependency between various players and systems on all sides of the referral process creates ample room for inefficiencies. For patients, a referral may mean yet another provider to see, a new diagnosis, or an escalation in care. This can be difficult to navigate on one's own, especially if the patient is unaware of the referral urgency or whether the referring specialist accepts their insurance. Meanwhile, primary care providers are responsible for triaging coordination between the specialist and the patient, and often lack insight into whether the patient followed the referral as intended, or whether the results were returned3.
Inefficiencies in a practice's referral system can have a drastic impact on a practice's ability to retain revenue, as well as on patient health outcomes. Healthcare systems lose on average 55%-65% of revenue to inefficient referrals4. With value-based care contracts becoming increasingly integral to practices’ funding structures, this out-of-network leakage is simply no longer an option. For patients, continuous engagement after the referral has been placed is essential to preventing a gap in the continuum of care and managing the patient's care acuity.
With greater awareness around who practices are referring to, how they're referring, and whether the process is simple and scalable, practices have the opportunity to address the three most prominent pain points in a referral management system – the communication gap, closing the referral loop, and accessing program insights – to establish a streamlined referral program. With the Azara DRVS Referral Management module, practices can seamlessly access actionable data that can be used to standardize the referral process, optimize staff resources, and evaluate the effectiveness of referral efforts.
Common Challenge #1 – The Communication Gap
With the separation of hospital- and office-based physicians and the elimination of physician lounges within hospitals, we are seeing a decline in “curbside” care5. This has created a siloed healthcare system that makes it increasingly difficult to gain clarity around and streamline communication between the patient, the provider, and specialists.
In part due to this breakdown in communication and continuity, up to half of all patients never follow through on their referral, which poses risk to both the patient and the practice6. One of the best ways to influence patient adherence is by establishing clarity around whether the patient or the provider is responsible for scheduling the appointment, then remaining engaged with the patient throughout their referral journey1. This, however, requires an understanding of what happens after the referral has been placed and accountability for transitioning patients to the next step in care. Thankfully, the referral reports available in the DRVS Referral Management module are designed to offer comprehensive insights into the referral itself, as well as the referral status.
Up to half of all patients never follow through on their referral, which poses risk to both the patient and the practice.
The All Referrals report, for example, surfaces a wealth of information, including the type of referral placed and who the referral was sent to. If documented in the EHR, the All Referrals report will surface the date the appointment was scheduled as well as the day the patient is scheduled to see the specialist. These plot points can help practices calculate their efficiency as it relates to getting patients into appointments and can be used to identify specialists with especially lengthy wait times. This visibility into supply (provider capacity) and demand (patient needs and preferences) can help practices build a more intentional and sustainable referral network.
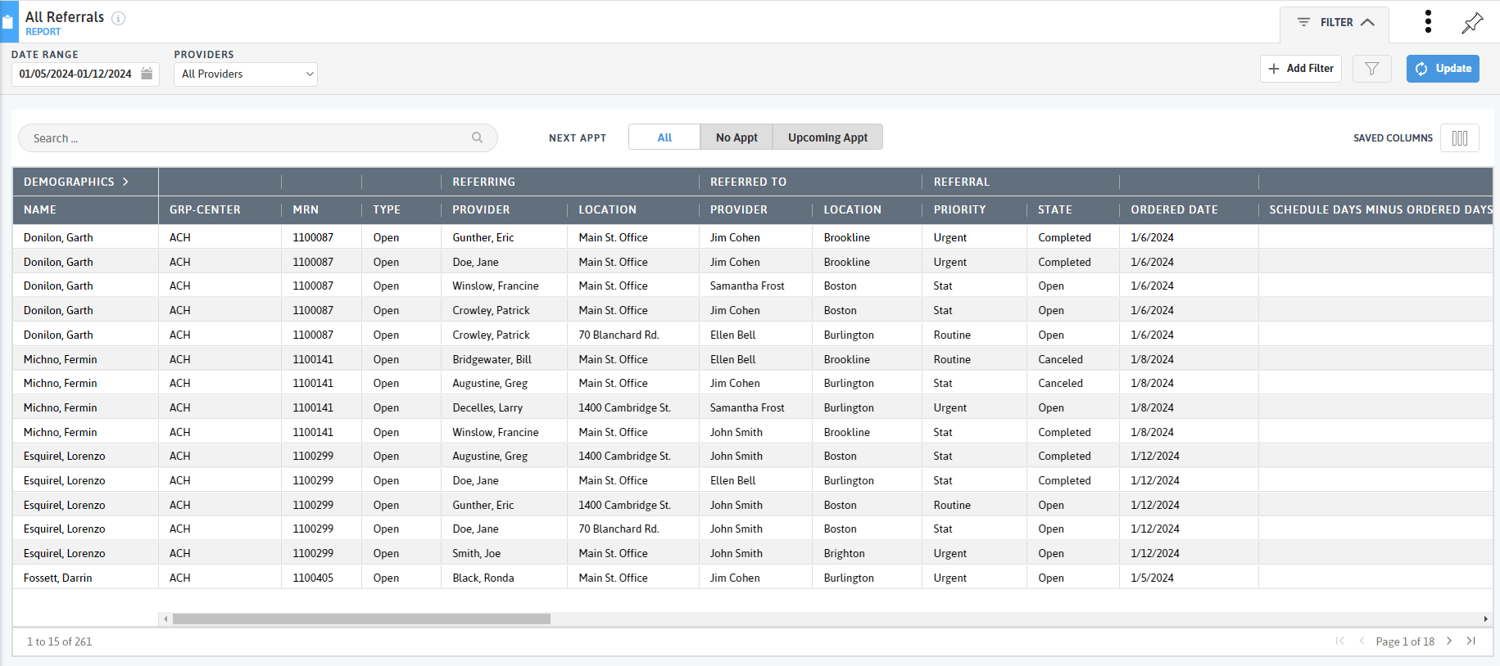
Other information highlighted in the referral reports includes the referral status: completed, canceled, deleted, or open. Open referrals will include a "Days Open" summary, supporting teams in prioritizing referrals to follow up on. When combined with robust workflows and standing orders, the referral reports in DRVS can be used to contact patients whose referrals are still open to better understand their barriers to care, identify referrals that should be sent to an alternate specialist with greater availability, and prioritize patients with "urgent" or "stat" referral statuses.
Common Challenge #2 – Closing the Referral Loop
While the referral reports in DRVS can be leveraged to proactively manage referrals, practices must also place special attention on closing the referral loop by identifying referrals that are open and do not have a returned specialist report. Retrieving this report typically presents a challenge to practices – 25% to 50% of referring physicians are unfamiliar with the eventual results of their referrals1. However, closing the referral loop is essential to facilitating care continuity, ensuring the patient receives the care they need, and managing organizational risk.
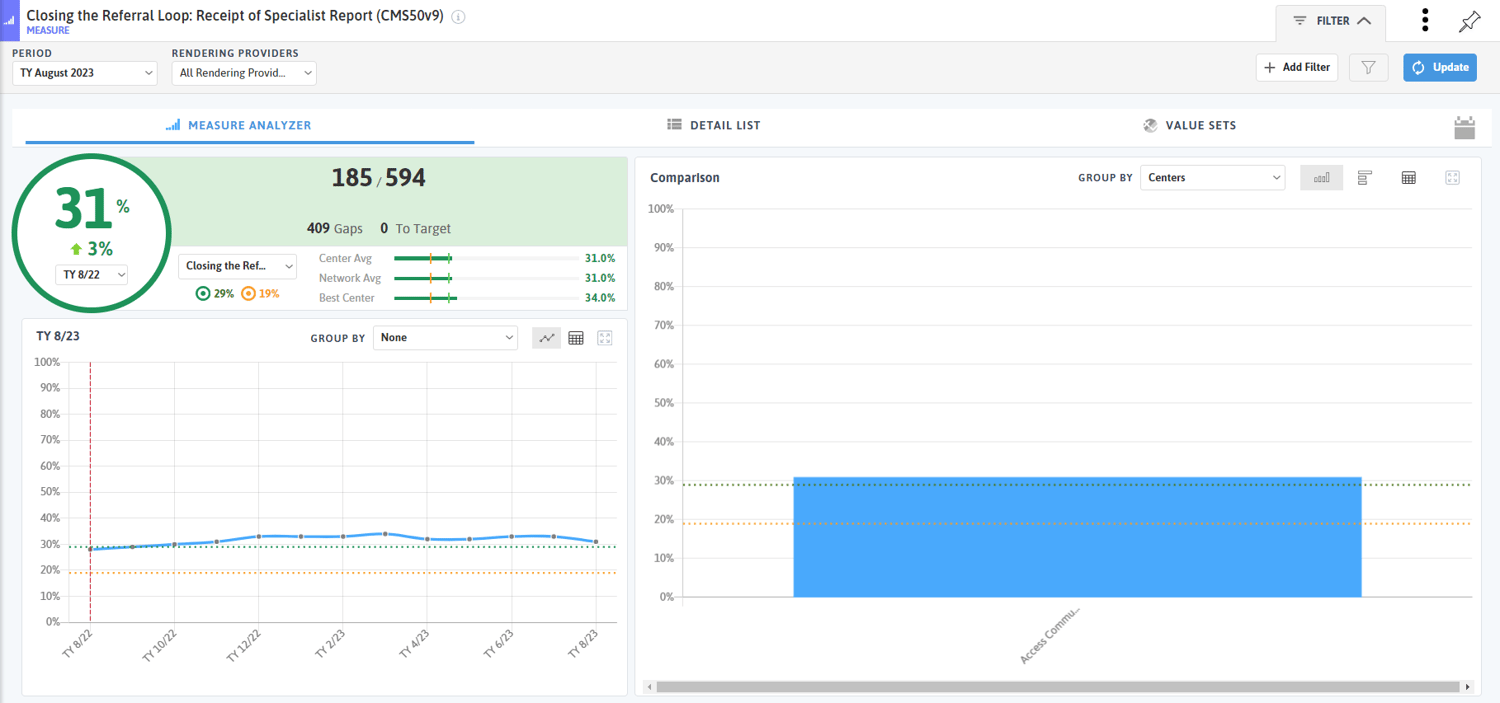
In DRVS, practices can use the Closing the Referral Loop: Receipt of Specialist Report measure to gauge the effectiveness of their specialist report retrieval processes and identify potential trends or opportunities for improvement.
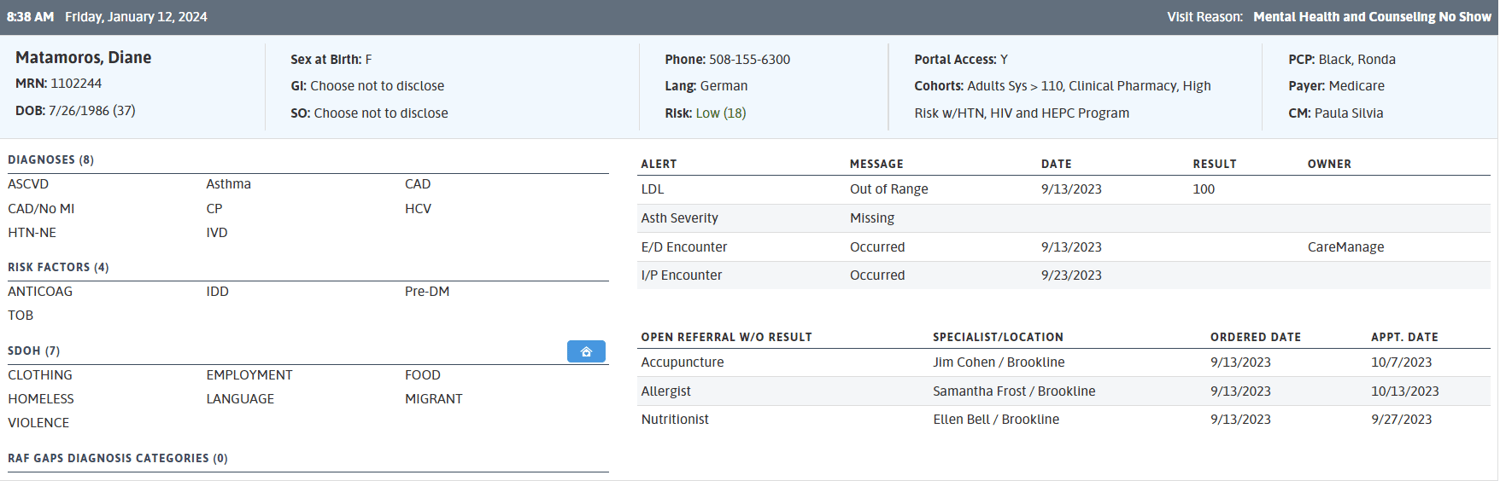
DRVS also surfaces open referrals on the Patient Visit Planning (PVP) report so that care teams can close the referral loop at the point of care. The Open Referrals section of the PVP will notify the care team with specifics about the referral, including the type, location, and date, so that they can meaningfully engage with the patient to understand whether they were seen by the specialist, the results of the visit, and what next steps must take place to get the results returned.
Common Challenge #3 – Accessing Program Insights
To break down the barriers that stand in the way of developing a high-functioning referral network, practices must be able to monitor high-level data and analytics that can tease apart its inner workings and bring light to its efficiencies and inefficiencies.
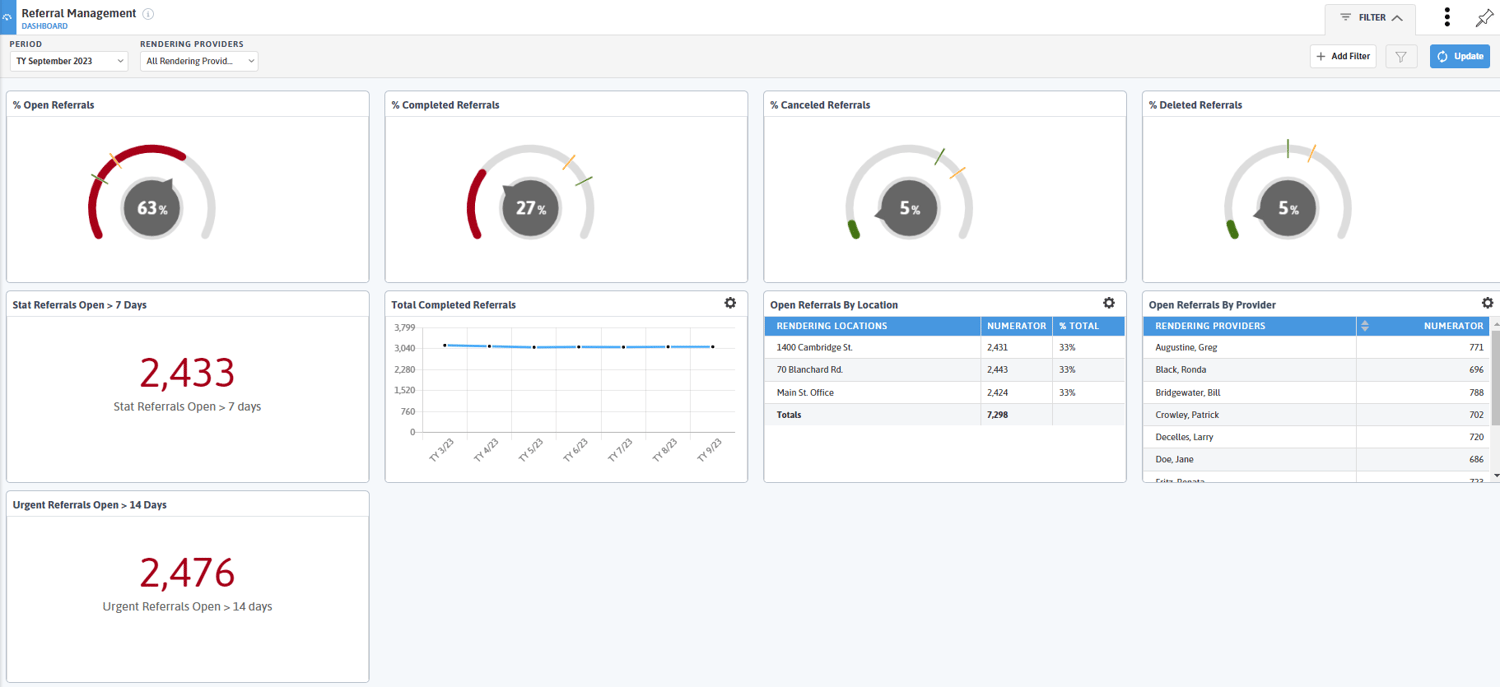
The DRVS Referral Management module comes equipped with a referral management dashboard that offers overarching data on the percentage of open, completed, canceled, and deleted referrals. Practices can assess the number of stat and urgent referrals open greater than 7 or 14 days, drawing attention to patients in need of immediate outreach, as well as workflow inefficiencies or resource limitations. The dashboard can be copied and tailored to evaluate referral patterns across care teams, locations, referral types, or priority populations, equipping the practice with actionable data that can be utilized to drive quality improvement. For guidance on how to build a compelling and valuable dashboard, read our blog Dashboards are Pretty Sweet: Data Visualization in DRVS.
Through the DRVS Referral Management module, practices have access to real-time data delivered to the appropriate care team members at the appropriate time. This even includes referral tracking and reporting that goes beyond medical and behavioral health specialty care to include referrals to community-based organizations and resources through integrations with findhelp and Unite Us. With functionality available to support everyone from the care coordination team, point-of-care staff, referral and coordination departments, and the quality team, practices can leverage this data to achieve greater efficiency in referral workflows, improve the quality of care delivered to patients, and deliver against value-based care contracts.
If your organization is leveraging the DRVS Referral Management Module in meaningful and creative ways to drive change, we’d love to hear from you. If you do not currently have the DRVS Referral Management module but are interested in learning more, please contact your client success manager or email solutions@azarahealthcare.com.
Contact solutions@azarahealthcare.com to learn more about how Azara Healthcare can empower your organization's population health and value-based care initiatives.
- https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1108675
- https://www.modernhealthcare.com/finance/three-ways-modernize-provider-referral-management-processes-keep-patients-network
- https://www.beckerspayer.com/payer/3-important-statistics-about-provider-referrals.html
- https://www.processfusion.com/en/the-role-of-referral-management-in-value-based-health-care/
- https://www.hfma.org/finance-and-business-strategy/population-health-management/61094/
- https://www.cms.gov/priorities/innovation/files/x/tcpi-san-pp-loop.pdf
Related Articles

Unlocking Value-Based Care Success: Why Supplemental Data Matters More Than Ever
Explore Insights
Turning Every Encounter into Value: How Azara's EHR Plug-In Elevates Risk Adjustment at the Point of Care
Explore Insights
