Cigarette smoking is one of the leading causes of preventable disease and death in the United States, accounting for about 1 in 5 deaths annually. And while smoking rates have declined in recent decades, 12.5% of U.S. adults currently smoke cigarettes, with higher rates among certain populations such as men, American Indian/Alaska Native individuals, those with a high-school diploma (or below), individuals with a household income less than 200% of the federal poverty level, and those with Medicaid insurance coverage.
An estimated 30.8 million adults in the U.S. currently smoke cigarettes and more than 16 million live with a smoking-related disease. The 2014 U.S. Surgeon General’s report on the Consequence of Smoking detailed the sobering statistic that more than 10 times as many U.S. citizens have died prematurely from cigarette smoking than have died in all the wars fought by the United States. In addition to lives lost, cigarette smoking cost the United States more than $600 billion in 2018, including more than $240 billion in healthcare spending.
Time to Quit
More than two thirds of smokers say they want to quit, and every day thousands try. But despite their desire, 43% of adult smokers who had seen a health professional in the past year reported NOT receiving advice to quit. From a Surgeon General report in 2020 on smoking cessation, there is sufficient evidence that behavioral and quitline counseling and cessation medication interventions increase cessation compared with self-help materials or no treatment. Even brief (less than 3 minutes) counseling from a provider increases quit rates.
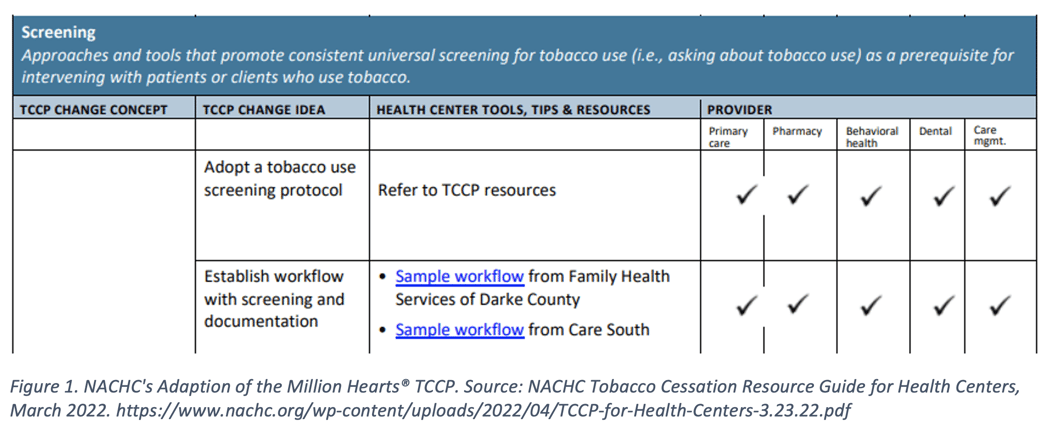
To assist healthcare professionals in all settings in improving care for patients who use tobacco, the Centers for Disease Control and Prevention (CDC) created a Tobacco Cessation Change Package (TCCP) with Million Hearts® tools to integrate tobacco dependence treatment into routine care delivery. The TCCP provides process improvements providers and healthcare organizations can implement and contains practical resources to increase the reach and effectiveness of interventions. The package was designed for all healthcare professionals, from primary care to specialties, from inpatient, outpatient, or behavioral health. Using five focus areas, Key Foundations, Equipping Care Teams, Screening, Treatment, and Referral and Follow-Up, the TCCP sets recommendations and resources for practices to use in developing systems to treat tobacco use and dependence.
Tobacco Cessation Programs in Action
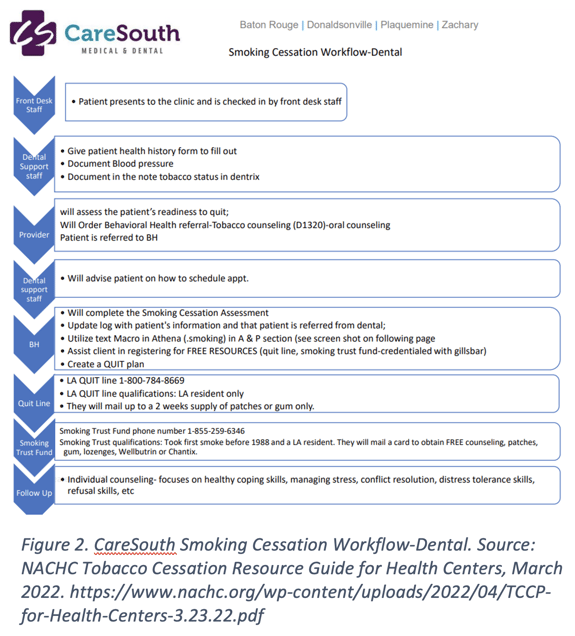
In partnership with the CDC, the National Association of Community Health Centers (NACHC) worked with Primary Care Associations and three health centers each from the Louisiana Primary Care Association (LPCA) and the Ohio Association of Community Health Centers (OACHC) to apply strategies recommended in the TCCP to the health center setting. This partnership identified dental and pharmacy staff as key assets who are especially well positioned to contribute to tobacco cessation success as part of a larger health care team. They also found success utilizing telehealth capabilities.
With the use of integrated care teams, the pilot health centers experienced success with the TCCP interventions, especially when paired with patient-relationship development and ongoing conversations. In their adaptation of the Million Hearts® Tobacco Cessation Change Package, NACHC, LPCA, and OACHC provided aligned resources specifically for health centers with the original TCCP structure and organization. They include tips and lessons learned, as well as the relevance for each specific provider-type.
The first change concept is to make tobacco cessation a practice priority. NACHC recommends creating an integrated team of dental, pharmacy, behavioral health, and primary care staff alongside quality, population health, and care management staff to review the current state of tobacco cessation at the organization and develop a plan to address identified gaps. This includes training the integrated care team staff and identifying and addressing patient barriers.
 Next, NACHC provides resources on equipping all staff to engage in tobacco cessation efforts. This includes resources on training and onboarding staff on tobacco policies, systems, and procedures based on their role. Training should also include billing practices and appropriate codes for services such as chronic care management and tobacco cessation counseling. In addition to training clinical staff, quality and population health staff should make tobacco cessation a quality improvement measure, tracking and sharing performance at the provider and practice level. They also recommend that primary care, behavioral health, and care management staff employ population health strategies—like risk stratification—to identify patients who use tobacco and are eligible for care management.
Next, NACHC provides resources on equipping all staff to engage in tobacco cessation efforts. This includes resources on training and onboarding staff on tobacco policies, systems, and procedures based on their role. Training should also include billing practices and appropriate codes for services such as chronic care management and tobacco cessation counseling. In addition to training clinical staff, quality and population health staff should make tobacco cessation a quality improvement measure, tracking and sharing performance at the provider and practice level. They also recommend that primary care, behavioral health, and care management staff employ population health strategies—like risk stratification—to identify patients who use tobacco and are eligible for care management.
At the point of care, the TCCP advises to create specific workflows and standing orders for tobacco screening and cessation counseling for each type of provider and care team (primary care, pharmacy, behavioral health, dental, and care management. The change package provides workflow examples from the participating health centers (see Figure 2). The project also found that incentives like gift cards and raffle drawings helped patients stick to their goals. In addition to incentives, personal outreach like a hand-written card and phone calls are appreciated by patients.
NACHC’s adaptation of the Million Hearts® Tobacco Cessation Change Package provides resources tailored to support health centers. Health centers’ integration of staff and providers is effective in the treatment and management of tobacco cessation efforts in their patients. PCA’s and HCCN’s also offer partnership when it comes to training and technical assistance.
Read Part 2 to learn different ways Azara tools can help support the change concepts of the TCCP.