We are all familiar with health awareness months and days—February is Heart Month, October is Breast Cancer awareness month, World HIV/AIDS day is held on December 1st every year. But one lesser known health awareness month I recently learned about is PTSD Awareness Month, which takes place every June. PTSD, or post traumatic stress disorder, is an anxiety disorder that develops in some people after a traumatic event such as combat, crime, an accident, or natural disaster. The U.S. Department of Veterans Affairs, a leading researcher on PTSD and traumatic stress, organizes PTSD Awareness Month events and works to raise awareness on PTSD and treatment options.
When many people think of PTSD, they often think of veterans— “shell shock” and “combat fatigue.” But PTSD can be the result of many types of trauma. In fact, approximately 3.5% of U.S. adults are impacted by PTSD every year (compare that to the 8.4% of US adults who suffer from a major depressive episode each year) and 6 out of every 100 people will have PTSD at some point in their lives. There is a dearth of data on PTSD in children and teens, but one study estimates that 5% of adolescents aged 13-18 meet criteria for PTSD (with higher prevalence in girls).
One growing area of research is the relationship between Adverse Childhood Experiences (ACEs) and developing PTSD and other mental health conditions. ACEs are potentially traumatic events—like emotional or physical abuse or neglect that occur in childhood. Additionally, unstable household environments, such as substance use or mental health problems and parental instability due to divorce or incarceration, can be traumatizing to children. In adults surveyed across 25 states, 60% reported they had experienced at least one type of ACE before age 18 and nearly 16% reported 4 or more ACEs. The risk of developing mental health disorders after ACEs is a dose-dependent relationship (meaning there’s higher risk of developing the condition the more ACEs one has experienced). This relationship is particularly true for PTSD.
In a world of increasing gun violence, devastating natural disasters, and other traumatic community events, it is important we incorporate ACE screening in routine primary care. In a literature review of 13 ACE studies, researchers found that most patients were willing to complete ACE screenings and parents viewed the screenings as a positive means of being identified for additional services. While at first hesitant on the administration of ACE screening due to timing concerns and lack of confidence, providers did not note any major workflow disruptions and felt that the ACE screenings helped develop a deeper patient-clinician relationship and led to better communication. Providers felt more confident if there were established workflows and processes in place and had sufficient resources to address high ACE findings.
If your practice uses the Patient Visit Planning report in DRVS, there are alerts you can enable that will fire to remind providers and care team staff to screen for adverse childhood experiences. In the core DRVS module, there are two ACE alerts: ACE Pediatric Screening, a yearly alert for patients 1 months to 17 years old and Adverse Child Event Screen, a lifetime screening for patients 18 and older.
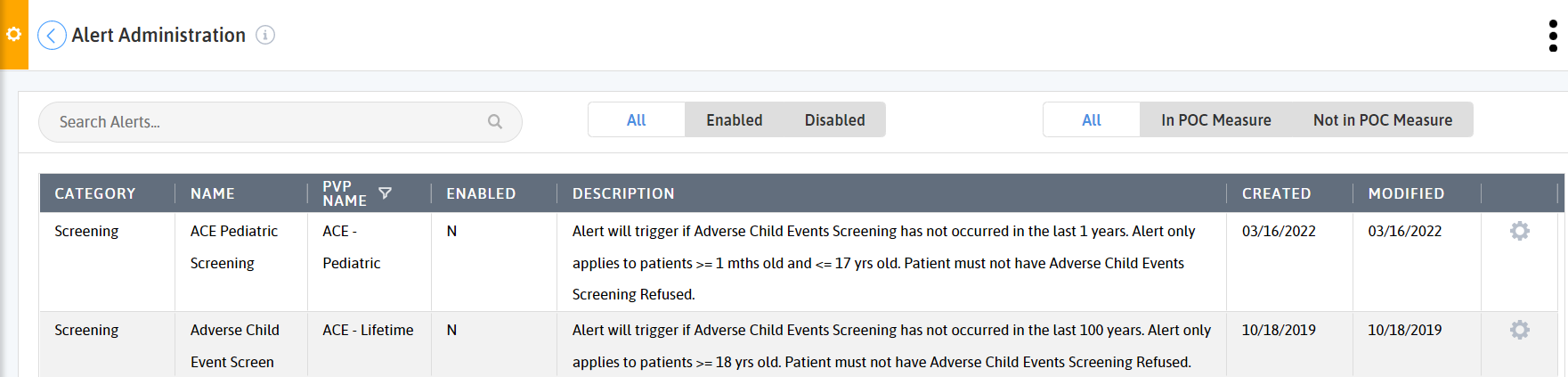
Both alerts are configurable, meaning you can change how often and for whom they fire.
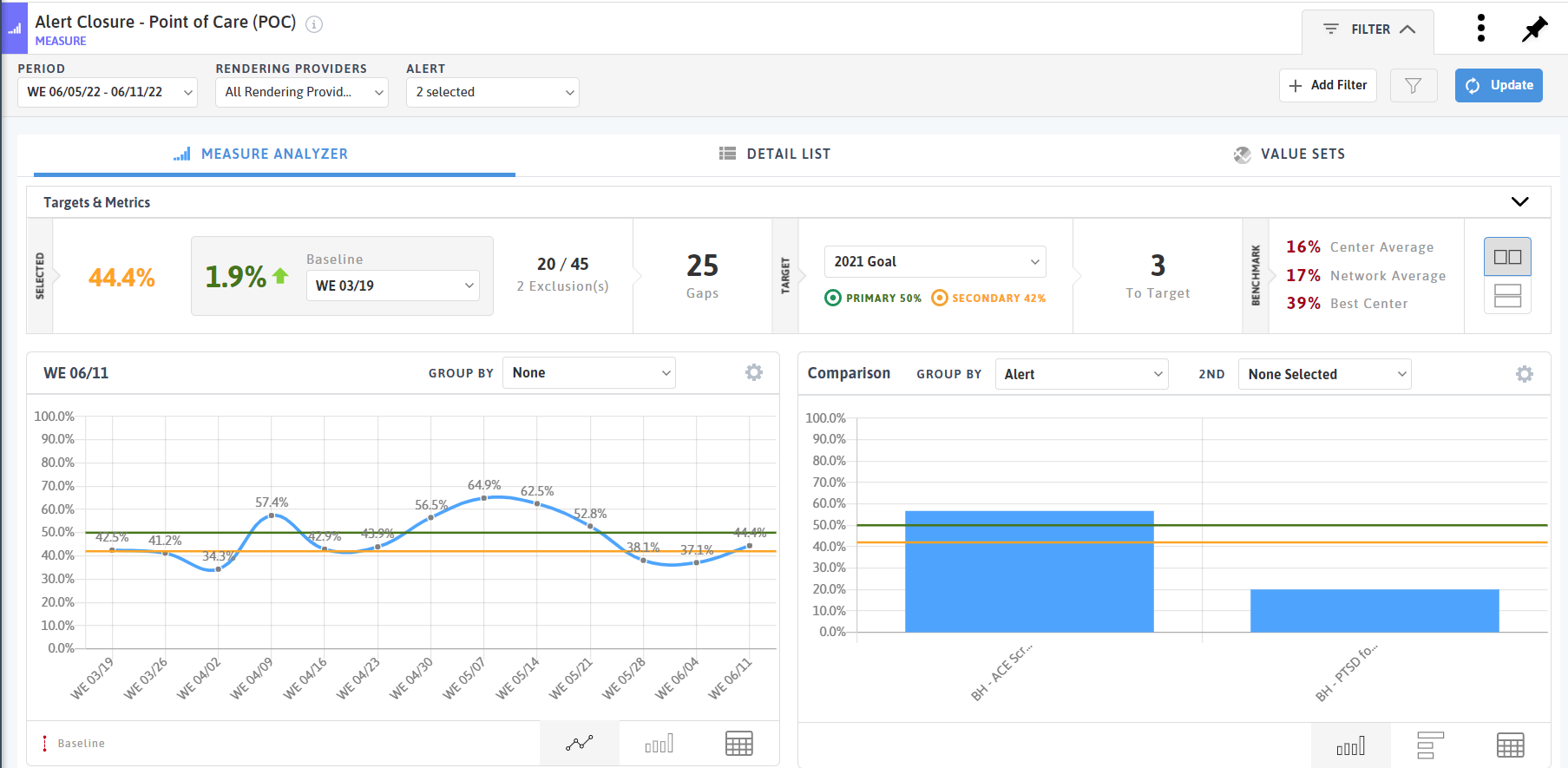
If enabled, users can track their ACE alert closure rate using the Alert Closure - Point of Care (POC) measure. You can group by alert and by rendering location or provider to see if the appropriate care teams are closing the alert and provide training and resources to those who aren’t.
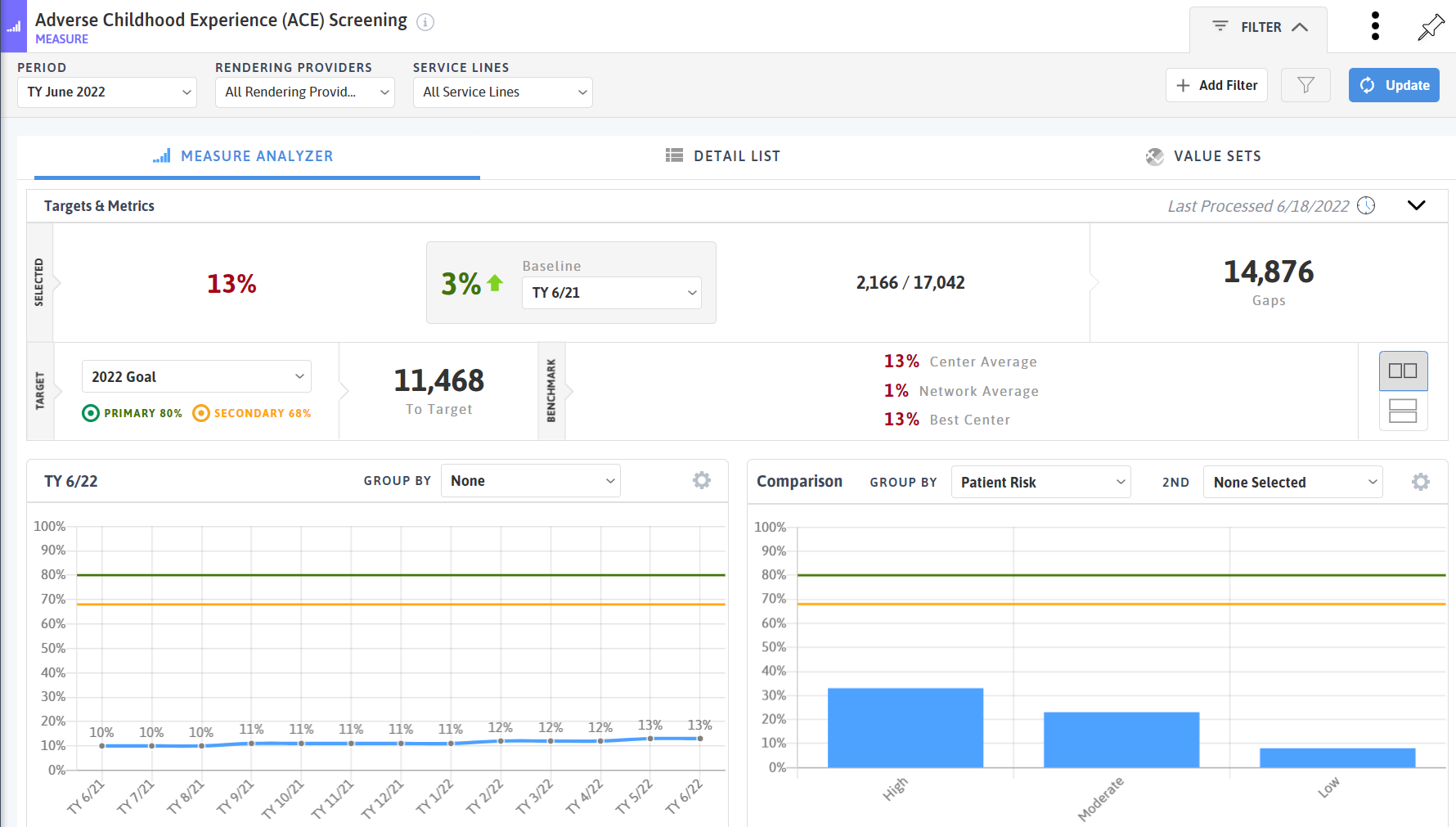
Increased alert closure can lead to higher screening rates overall. These trends can be reviewed in the Adverse Childhood Experience (ACE) Screening measure. The measure allows users to see trends in screening rates period over period, and the detail list contains the patients’ ACE screening date and score.
.png?width=188&name=MicrosoftTeams-image%20(15).png) For practices interested in expanded behavioral health reporting, there is a Positive ACE Follow Up alert that looks for a PTSD screen to occur after a positive ACE screen and a PTSD Screen After ACE Screen measures that allows you to track the same criteria.
For practices interested in expanded behavioral health reporting, there is a Positive ACE Follow Up alert that looks for a PTSD screen to occur after a positive ACE screen and a PTSD Screen After ACE Screen measures that allows you to track the same criteria.
Across DRVS, users can add the ACE Score filter and grouping option to many different reports and measures like the 2022 UDS CQMs and new Patient Retention measures.
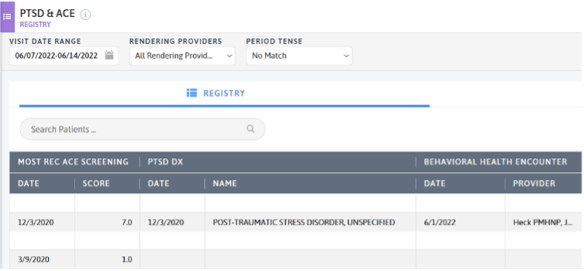
In addition to alerts, users can create a custom registry using data elements of ACE screening, PTSD screening, PTSD diagnosis, and behavioral health encounter. You can add other data elements like chronic disease diagnoses, most recent vital signs, and social determinants of health to gain a deeper understanding of challenges the patient might be facing.
Outside of Azara tools, connect with community organizations to provide resources for patients with positive ACE screenings. Organizations like Brain Health Bootcamp provide evidence-based mental health education for students and families. FindHelp (previously known as Aunt Bertha) enables their users to build networks of social care to support their patients and communities.
When it comes to PTSD, there are treatments available. Both trauma-focused psychotherapy and medication are proven to treat PTSD. There is no shame in seeking help to manage your PTSD. If you or a loved one are suffering from PTSD, reach out to your provider or find additional resources online.
Related Articles

Turning Every Encounter into Value: How Azara's EHR Plug-In Elevates Risk Adjustment at the Point of Care
Explore Insights
Value-Based Care Foundations Part 2: A New Chapter in Risk Adjustment
Explore Insights
