Missouri Primary Care Association
Missouri FQHCs use Statewide Data-driven Performance Improvement to Boost Hypertension Control
IN BRIEF: The Missouri Quality Improvement Network (MOQuIN) undertook a Health Resources and Services Administration (HRSA) Health Center Controlled Network (HCCN) grant-funded initiative that aimed to help the state’s federally qualified health centers (FQHCs): adopt, implement, and upgrade HIT for Meaningful Use incentives, obtain the incentives, and leverage data for quality improvement in a Patient-Centered Medical Home (PCMH) environment.
Participating FQHCs agreed to work for three years to improve four measures, all with aggregate Missouri targets against which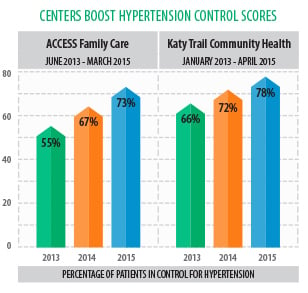 they measured success. Significant across-the-board improvement on two of the targeted measures – hypertension control and diabetes A1c control proved to be elusive, with most centers’ performance plateauing after years of improvement. However, two centers demonstrated significant hypertension control gains. Those centers – Katy Trail Community Health and ACCESS Family Care – met and exceeded the targets due, in part, to Azara DRVS tools enabling them to mine their patient data, to identify the causes of poor performance, and to test and measure the efficacy of strategies for improvement. Powered by data, these centers were able to use their innate quality improvement and operations skills to implement the strategies and provide the leadership and training necessary to ensure that all teams adopted the successful interventions they identified.
they measured success. Significant across-the-board improvement on two of the targeted measures – hypertension control and diabetes A1c control proved to be elusive, with most centers’ performance plateauing after years of improvement. However, two centers demonstrated significant hypertension control gains. Those centers – Katy Trail Community Health and ACCESS Family Care – met and exceeded the targets due, in part, to Azara DRVS tools enabling them to mine their patient data, to identify the causes of poor performance, and to test and measure the efficacy of strategies for improvement. Powered by data, these centers were able to use their innate quality improvement and operations skills to implement the strategies and provide the leadership and training necessary to ensure that all teams adopted the successful interventions they identified.
At the Missouri Primary Care Association (MPCA)/MOQuIN level, Quality Coaches were easily able to identify Katy Trail and ACCESS as successful outliers by using the comparative analytics in Azara DRVS. As a result, they asked Katy Trail and ACCESS to share their hypertension success stories with the other Missouri FQHCs during one of the MOQuIN meetings. The bi-monthly forums gather representatives from the 28 centers that are MPCA members, and provide a valuable forum for their staffs to hear about the latest quality initiatives, to share best practices and to learn the most effective methods for using DRVS.
THE STORY: MOQuIN, a subset of the MPCA’s Center for Health Care Quality, selected four Uniform Data Set (UDS) measures – hypertension control, diabetes A1c<7, childhood immunizations and cervical cancer screening – as the targets for improvement. MOQuIN leaders expected that the hypertension and diabetes A1c scores would be the easiest of the four measures to boost since they had seen past improvement in them due to Plan-Do-Study-Act (PDSA) change testing interventions. The opposite proved to be true: despite continued emphasis and change testing, hypertension and diabetes performance remained about the same at the aggregate level, while cervical cancer and childhood immunization measures jumped.
However, something within the center-wide data caught MOQuIN’s attention.
“There were a few notable exceptions to the two measures that flat-lined,” said Susan Wilson, COO at MPCA. One of the examples is: “Two centers improved significantly on hypertension, and they are paving the way for some best practices that other centers can adopt.”
Katy Trail Community Health and ACCESS Family Care stood out from the pack. When MPCA staff talked with the two standout centers, the narrative revealed the centers owed their hypertension management success, in part, to their ability to analyze their patient data in DRVS, both in aggregate and at the individual patient level, and in their ability to implement improvement programs that addressed the gaps or concerns identified by the analysis.
Both FQHCs used the Azara DRVS data analytics and reporting tool to aid their hypertension control improvement efforts. With DRVS, Katy Trail and ACCESS started with the aggregate statewide performance and compared their own centers’ performance with that of their peers. After that, they drilled into their performance data to look for patterns at the location, provider, or health disparity levels for clues that might yield theories for further tests of change. Because of the capacity to look at the data over time with trend lines and other visualization tools, the centers were able to identify likely barriers to improved care and to develop effective change interventions (such as new care delivery workflows) that boosted performance.
MOQuIN, which comprises 28 FQHCs, uses DRVS to provide center-to-center data comparisons. The centers evaluate key quality measures by comparing their performance with their peers. Because of this comparative capacity, DRVS also provides teaching opportunities: centers that score well on certain measures can share their best practices with centers that need to improve their scores. This sharing occurs center to center, since MPCA centers chose to use a transparent approach and have their center names identified in the DRVS tool; practices can readily tell which centers are performing best. They can reach out to a well-performing center to find out what the center may be doing differently. In addition, the best practices are identified and shared with participants at the MOQuIN meetings.
Katy Trail and ACCESS are among the centers that participate with enthusiasm at the MOQuIN meetings. The forums assemble participating FQHC staff in a day-long event that provides insights and information that can help centers use their data to its full potential and remove barriers to improved care delivery. MOQuIN also provides updates on state and federal programming, grants, and other critical areas to prepare for in the ever-changing health care environment.
Center’s Blood Pressure Rises as Its Hypertension Scores Fall
ACCESS Family Care had traditionally performed well on hypertension measures, with 64%-67% of its patient population in control. But at a certain point in time, something unexpected occurred.
“In June 2013 we noticed a significant decline,” said Venice Green, the center’s quality assurance manager.
In fact, their data showed their performance had dipped to 55%. Minor fluctuations in quality measures are normal, but ACCESS’s steep drop baffled the center. Green and her team dug into the data and learned that the drop coincided with the introduction of automated vitals testing devices that include a blood pressure check function. ACCESS had previously used manual cuffs to check blood pressure, but began using the machines to improve workflow efficiency.
In response to the center’s drop in hypertension control, they decided to test a change based on the analysis of their DRVS data. One of its four sites switched back to the manual cuffs; three clinics continued to use the machines and conducted a comparison study to identify any discrepancies in the equipment. Hypertension control improved at the site that returned to the manual cuffs, while scores at the other sites continued to decline.
ACCESS concluded that something associated with the machines must have been related to the drop in hypertension scores. Green said staff determined that the highly-sensitive machines were not the right fit for the center’s blood pressure testing needs because medical staff members typically speak with patients when checking their vital signs –including blood pressure. Their theory was that the interaction prevents patients from reaching an adequately rested position, which can cause elevated blood pressure readings. So it was not the fault of the machines, per se, but ACCESS felt the challenge of trying to get patients adequately rested before using the machine was not worth the effort.
The center switched back to the manual cuffs. It also embarked on an intensive training program that aimed to ensure all medical assistants and nurses took patients’ blood pressure in a consistent manner.
In addition, ACCESS’ investigation of its hypertension drop revealed that blood pressure rechecks, meaning a second or third blood pressure check following a high one, were not being recorded in the appropriate field within the center’s EHR. This issue contributed to their decreased scores. ACCESS identified this issue by reviewing a series of patients which DRVS data evaluated as “not in control,” meaning their blood pressure was outside of the parameters. They noticed the data in DRVS did not reflect the re-check readings they could see in their EHR. But why? They also discovered their re-check blood pressure readings were being documented in a different EHR field, one from which DRVS was not pulling data. This was not how staff had been trained to record blood pressure in the EHR. All readings were supposed to be recorded in the same field that saved all the readings taken for a patient during an encounter. When entered into the correct field, the patient’s most recent blood pressure reading would accurately reflect the re-checks.
As a result of these interventions, hypertension control numbers bounced back to 67% during the next few months and peaked at 73% in March 2015.
Breaking Rules Produces Hypertension Win
Katy Trail Community Health also ranked among Missouri’s best hypertension control performers, but improving its performance on the measure, and therefore patient care, first required the center to realize there was an even larger hypertensive patient population in its midst than it had believed existed.
“You don’t feel sick from high blood pressure,” said Pam Hirshberg, COO at Katy Trail. “It’s a diagnosis that does not bring patients to the center.”
In fact, Million Hearts, a U.S. Centers for Disease Control & Prevention initiative, estimated in 2010 that 29% of hypertension in patients goes undiagnosed. That year, Hirshberg attended a conference in Washington, D.C. where a speaker from Million Hearts spoke to the group and she learned of hypertension’s undiagnosed nature. Patients do not complain about hypertension (the effects of the disease often do not manifest until later in life), and care providers can miss hypertension if they are focused on treating other conditions that have more overt symptoms, such as diabetes or chronic heart disease.
The health center implemented rigorous protocols for blood pressure taking, and specially-tailored provider communication alerts to help ensure that all patients get evaluated for hypertension if their blood pressure is high, regardless of the reason for their visit. Katy Trail also works to ensure hypertensive patients receive appropriate follow-up care. That begins with adding the hypertension diagnosis to the patient’s problem list, so that he or she will show up on the Patient Visit Planning Report alerts, registry reports, or performance measures, to support population health management.
DRVS provides Katy Trail with a robust data analytics tool that allows them to evaluate different aspects of care delivery to look for opportunities. Hirshberg said the center uses it to view performance measures by comparing teams of providers –as well as individual providers at the center – in order to discover outliers that indicate training gaps or blind spots, as well as to harvest best practices for sharing at provider meetings.
To implement a successful program, the center needed to assemble a team with the correct mix of skills to interact with the data as well as to test and implement changes in practice. Morgan Lynch is Katy Trail’s clinical data coordinator. She handles much of the complex data and reporting the center uses to collect and analyze its metrics; Hirshberg has the authority within Katy Trail’s hierarchy to adopt programs and initiatives that can improve care.
“I believe it’s the combination of the two of us working together that makes the difference,” said Hirshberg. There’s no question: they are a powerhouse team together because each has passion and expertise in her area of focus.
Katy Trail started its hypertension improvement efforts in 2012. By the next year, its control rate had jumped to 66%; in April 2015, it had climbed to 78%.
Implementing the program that made the difference required Hirshberg to alter her management approach. She already knew and emphasized the value of standardization in certain areas. However, she came to understand that care teams are unique and they work most effectively when workflows are tailored to their preferences, when appropriate. Some of the physicians prefer to receive a quick text message to alert them that a hypertensive patient is waiting in an exam room; others respond to simple visual cues. In the latter cases, a medical assistant or nurse places a red heart on the exam room door, indicating the patient has hypertension.
“I had believed that every care team should function the same,” she said. “I broke my own rule that all provider teams need do things the same way – and it worked.”
Centers Assemble for Deep Data Dive
Every other month, representatives from Missouri’s 28 health centers gather to discuss quality initiatives, to share best practices for improving care, and to learn how to maximize the use of their data. Each MOQuIN meeting, which lasts several hours, includes a segment that targets aspects of DRVS that can benefit the centers, including tips on how to mine data.
The meetings also include a segment for centers to present their success stories to the group. Katy Trail and ACCESS shared their hypertension control efforts during one of these segments.
“We look at their measures and then we invite them to come in and tell us what their secret is. In this case, we found two very different approaches,” said MPCA’s Wilson.
Senior-level operations staff members from the health centers are encouraged to attend the meetings so that they can learn firsthand the benefits of quality initiatives for their centers.
“We really do have a wonderful collaboration with the other FQHC’s,” said ACCESS’ Green. “It breeds success when we can come together and share ideas.”
Katy Trail’s Hirshberg said health centers benefit from the MOQuIN meetings the most when they bring the right mix of staff. High-level staff members who have the authority to approve significant operational changes are needed at the meetings – in addition to the quality staff – so that they can see how testing different initiatives might boost center performance. Leadership buy-in is critical to the adopting of new initiatives, she said.
ACCESS and Katy Trail are prime examples of health centers participating at the highest caliber in the MOQuIN meetings, with the right staff present to make decisions and allocate staff, but also truly using data to drive the improvement of patient care. The presentation of their work to their peers has also sparked related initiatives at other health centers in the collaboration, including applying some of the ideas and techniques used, to the other measures of focus. More improvement is on the horizon for the Missouri HCCN, MOQuIN, its participating health centers, and most importantly, their patients.
